Snoring & Obstructive Sleep Apnoea (OSA)
Snoring key points:
- Snoring is extremely common resulting from partial collapse of the soft tissues around the upper airway with a resulting “vibrating” of the soft tissues leading to the snoring sound.
- Snoring is often associated with episodes of obstructive sleep apnoea (OSA).
- Snoring is a frequent cause of bedroom-stress due to difficulty of partner sleeping.
- Snoring often results in a sore throat and dry mouth.
- Snoring is made worse by drinking alcohol and taking sedatives.
- Reports indicate 95% reduction in snoring using an oral appliance called a mandibular advancement splint (MAS).
Obstructive Sleep Apnoea (OSA) key points:
- Apnoea literally means cessation of breathing. These episodes of OSA may last from a few seconds to over a minute and they result in poor quality sleep and a drop in the level of oxygen in the blood.
- OSA is a potentially serious condition in which people stop and start breathing repeatedly during sleep. This interrupts the pattern of deep sleep during which the brain recuperates from the day’s activities.
- OSA affects 1 in 3 people and affects over 100 million people worldwide (WHO figures).
- There is an established link between OSA and several serious medical conditions including diabetes, obesity, depression, raised blood pressure, heart disease and stroke.
- OSA is most common in overweight men but can be found in all ages, irrespective of obesity and in both sexes.
- Often patients with OSA are unaware of their condition.
- Patients with OSA often feel tired during the day and are more likely to suffer workplace related accidents and motor vehicle accidents than other people. They are frequently grumpy and often can’t think straight due to their underlying tiredness.\
What is OSA?
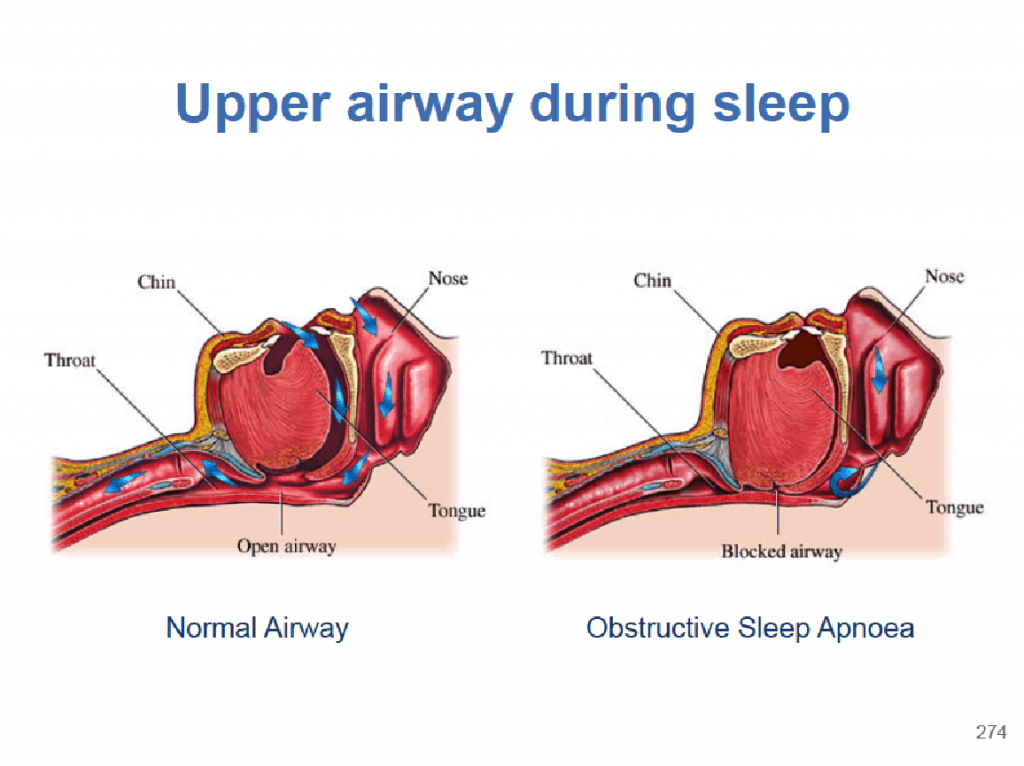
The airway behind the tongue, called the posterior airway space, collapses due to muscular relaxation that occurs during deep relaxing sleep. When taking a breath, the soft tissues of the airway either partially or completely collapse, obstructing the airway and preventing air entering the lungs.
A partial obstruction results in reduced airflow, known as hypopnoea and complete obstruction leads to cessation of airflow completely, known as apnoea. From the anatomical diagram below, the tongue falls back blocking off the airway.
An oral splint can be worn to maintain the forward position of the lower jaw (mandible) and this helps to maintain tongue support preventing the collapse of the soft tissues closing off the posterior airway space. Such a splint is called a Mandibular Advancement Splint (MAS). Patients suffering more severe OSA may require a continuous positive airway pressure (CPAP) machine to use at night. However patient acceptance with MAS is far higher than with CPAP.
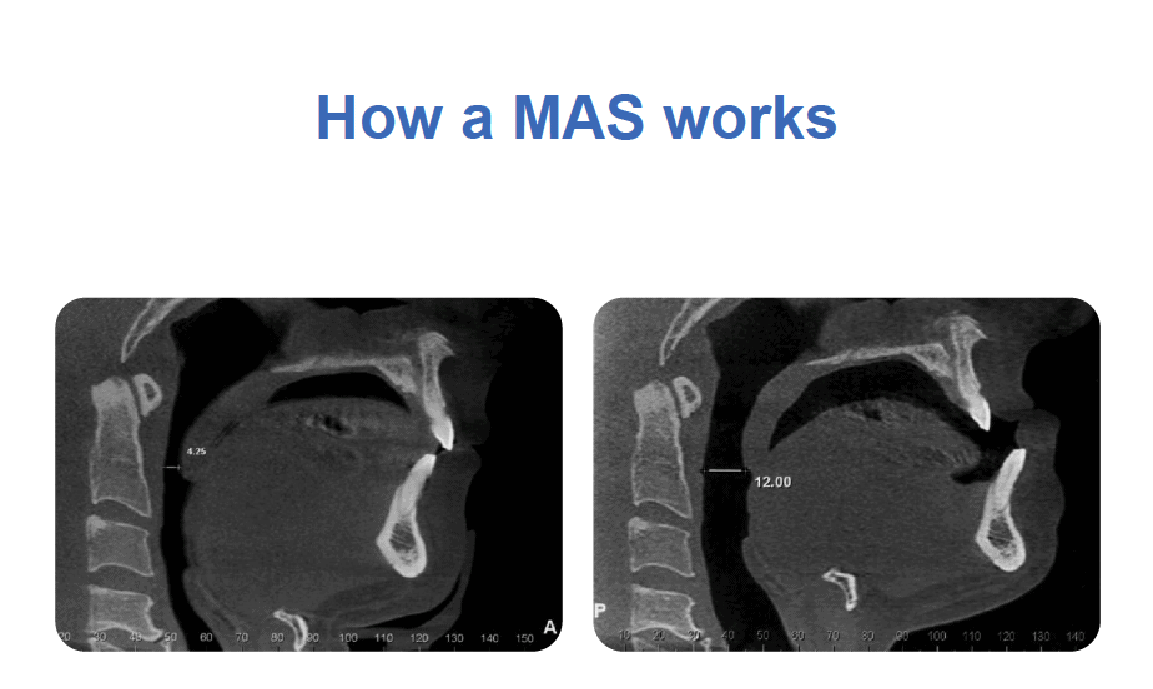 Diagrams and X-rays courtesy of Dr Harry Ball
Diagrams and X-rays courtesy of Dr Harry Ball
The X-rays show how on the left there is only a very narrow airway (4.25mm) while the lower front teeth remain behind the upper teeth in what is a normal position. In the X-ray on the right when the lower teeth are brought forward, the mandible that has the tongue attached to it, brings the tongue forward and in so doing, it opens up the space behind the tongue, (posterior airway space) increasing the space to 12mm. This is the basis of the success of the MAS as a treatment for OSA and snoring.
The effect of hypopnoea or apnoea
With reduced, or cessation of breathing, the cells of the body quickly use up the available oxygen in the blood leading to a fall in the oxygen saturation of the blood and an increase in the level of carbon dioxide carried in the blood.
Usually it is the small increases in carbon dioxide that drives the body to breathe. However if the airway is obstructed by soft tissue, breathing cannot take place and the patient‘s effort to try to breathe results in their becoming more awake, often waking with a feeling of panting, gasping or choking. This partial waking from sleep is described as an arousal. This lightening of sleep can lead to sudden complete wakefulness or simply result in a poorer quality of sleep. This regular arousal throughout the night results in inadequate rest for the body’s healing, repair and refreshment to take place.
These periods of hypopnoea or apnoea can occur many times every hour and is measured by the sleep study as the Apnoeic Hypopnoeic Index (AHI). With repeated apnoea, sleep is so badly affected that patients fail to recharge their batteries at night and become increasingly tired, irritable and find they have very poor concentration during the day. An AHI of more then 30 per hour is considered severe.
What are the symptoms of OSA?
The most common symptom of OSA is snoring. Often patients who suffer from OSA snore very loudly and this can result in pressure being placed on personal relationships with the sufferer having to sleep in a separate bedroom.
Cartoon courtesy of Dr Harry Ball
OSA can also result in the patient waking up feeling as if they are choking or gasping for air. OSA sufferers frequently perform erratic leg movements while asleep and may wriggle their legs constantly during the day, a condition known as “restless legs syndrome”.
Patient with OSA often complain of daytime tiredness. They may fall asleep after lunch, when sitting reading, while in a cinema or other public place, even in front of the computer or when having a conversation. Some even fall asleep at the wheel when driving. Research has shown that OSA sufferers are 4 times more likely to have a road accident than other people.
Who suffers OSA?
People of all ages and both sexes can suffer from OSA. It can affect healthy fit individuals but more often affects obese middle-aged people, more commonly men. However, women after menopause are also frequently affected.
How to diagnose OSA
The only reliable method of diagnosis is by means of a “sleep study”, also called “polysomnography”. This can be arranged in a sleep medicine laboratory or at home, both through referral to a sleep medicine specialist or through your GP
These studies can be performed with different levels of equipment from a level 1 study measuring every parameter to a level 2 study measuring a large number of parameters, both being conducted in a sleep laboratory. Level 3 and 4 studies can be arranged at home in your own bed, the latter often being more representative of the normal situation.
Once the study has been completed and all the data collected digitally, it can be analysed by a sleep medicine specialist and a “polysomnography report” is written that will detail the severity of sleep disorder from which you are suffering.
A questionnaire has been developed to help predict those patients most likely to suffer from OSA. The STOP-BANG questionnaire has been found to be effective.The letters STOP-BANG indicate the risk factors.
S Snore: Do you snore loudly?
T Tired: Are you tired and sleepy during the day?
O Observed: Has anyone observed you stop breathing when you sleep?
P Pressure: Are you being treated for or do you suffer raised blood pressure?
B BMI: Is your BMI over 35?
A Age: Are you over 50 years old?
N Neck circumfrance: Is your NC >40cm?
G Gender: Are you male?
If STOP-BANG is >3 then there is a high chance of OSA existing and if <3, OSA is unlikely.
How is OSA treated?
Weight loss
Often the first suggestion is for obese patients to try to loose weight. Even 10% reduction in body weight can have a profound effect on the degree of OSA or hypopnoea resulting in a 26% reduction in the respiratory disturbance index. However, weight loss is not always accompanied by reduced severity of OSA or snoring.
CPAP
Following weight loss, there are two ways to treat OSA. Historically, continuous positive airway pressure (CPAP) has been used. This relies on the patient tolerating one of a number of mask designs to cover either the nostrils alone, the entire nose or the nose and mouth, to allow air to be blown into the airway under positive pressure to inflate the airway to stop it collapsing. This works but many patients find the masks difficult or uncomfortable to wear and find they wake during the night with the mask not fitting correctly due to rolling onto the side and a noisy escape of air taking place. This results in poor acceptance in some patients.
Oral devices
Over recent years oral devices have been developed to hold the lower jaw forward to a degree that reduces the tendency of the tongue to relax back against the posterior airway wall sealing off the airway. These oral appliances are called various names; most commonly they are referred to as mandibular anterior positioning splints (MAS), of which there are many designs. No single design is superior to all others. Many have benefits and may suit a particular patient.
Many designs of MAS exist and a number work well in different patients, however for the best result, they must be custom made for the patient to achieve a stable fit ensuring the appliance cannot move on the teeth during the night. This is one of the main shortcomings of “off the counter” appliances that can be purchased from stores. They must also be adjustable allowing the degree of anterior positioning of the lower jaw to be accurately set to the point at which snoring and OSA cease. It is the latter point that is most essential from a health point of view. Those appliances bought from stores are generally not adjustable, another one of many short-comings.
Some science to back it up!
Research now supports the use of MAS for the treatment of snoring and mild to moderate OSA (Fernanda et al. J Clin Sleep Med 2009: 5(3)). CPAP generally remains the gold standard for the treatment of severe OSA but not all patients are able to tolerate CPAP. For those patients research is now suggesting that even in severe OSA, MAS therapy can be successful (Katz et al, J Clin Sleep Med 2015: 11(7); 773-827. Clinical practice guideline for the treatment of obstructive sleep apnoea and snoring with oral appliance therapy: An update for 2015)
A landmark research study clearly demonstrated that “state-of-the-art” oral appliances were overall equivalent to CPAP in terms of improving blood pressure, quality of life, sleepiness and the apnoeic-hypopnoeic index (AHI) and was considered superior to CPAP in 4 of 8 quality of life measurements (Craig et al. Health outcomes of CPAP versus oral appliance treatment for obstructive sleep apnoea. Am J Resp & Crit Care Med February 2013). This suggests that MAS should not only be used for patients suffering from mild to moderate OSA, and for those in the group suffering from severe OSA but who cannot use CPAP. The performance of MAS in the treatment of OSA in all patients should therefore be considered as good as CPAP and therefore suitable as a first line therapy equally as effective as CPAP.
More recent research by Dr Carol Lang at the University of Adelaide has demonstrated a clear link between OSA and depression in men. Male OSA patients should be questioned regarding any experience of loss of interest in work, hobbies, family or increasing sadness. If there is any suspicion of depression they should be advised to speak to their GP. Another useful resource is the Beyond Blue website (beyondblue.org.au). They may find this useful to help them accept that they may need professional support.
Avoiding OSA?
In order to reduce the chance of suffering from OSA, patients who have a tendency to snore should abstain from smoking, minimise alcohol intake, particularly in the evening, as this further relaxes the muscles and contributes to snoring and OSA. They should also avoid caffeine at night and avoid eating a large meal late in the evening.
OSA patients should avoid taking sleeping tablets but if they have been prescribed, then the GP must be involved in any decision to change your medication regime or discontinue any medication.
What possible side effects exist?
Some people experience a change in the position of some of their teeth. This varies from patient to patient. These changes cannot be predicted and some changes can be undesirable but on questioning, patients considered these occlusal changes as acceptable in view of the positive results experienced in treating snoring and OSA.
Temporo-mandibular disorder has also been reported in some patients wearing MAS. Approximately 12% of patient treated with MAS experienced this side effect (Dr Alan Lowe – Presentation at the Meeting of the American Academy of Dental Sleep Medicine 2007, Minneapolis, USA). This therefore supports the need for 6-12 monthly review of patients receiving treatment for OSA or snoring using MAS therapy.
Contact the friendly team at NQ Surgical Dentistry today on (07) 4725 1656 or call in to see us at 183 Kings Rd, Pimlico QLD 4812
BOOK AN APPOINTMENT
CALL US TODAY
07 4725 1656
